HPV - new infection or reactivation?
Last edited 08/2020 and last reviewed 07/2022
Older women should not be told that detection of HPV always indicates a new infection, but rather that detection of HPV could result from an infection acquired many years ago (1)
- determining that an HPV infection has cleared should not be based on 1 or 2 negative test results, as nearly all studies have done
- evidence suggests that type-specific HPV can be detected again after a long period of apparent clearance
A study undertaken by Ermel et al examining HPV 16 detection (2):
- sample of 27 adult women with known HPV 16 detection during adolescence was assessed for HPV 16 redetection. A comparison of the long control region (LCR) DNA sequences was performed on some of the original and redetected HPV 16 isolates.
- median age at reenrollment was 27.5 years (interquartile range of 26.7-29.6). Reenrollment occurred six years on average after the original HPV 16 detection. Eleven of 27 women had HPV 16 redetected. Some of these HPV 16 infections had apparently cleared during adolescence. LCR sequencing was successful in paired isolates from 6 women; in 5 of 6 cases the redetected HPV 16 isolates were identical to those detected during adolescence
- study authors concluded that
- HPV 16 may be episodically detected in young women, even over long time periods. HPV 16 redetection with identical LCR sequences suggests low-level persistent infection rather than true clearance, although newly acquired infection with an identical HPV 16 isolate cannot be excluded. However, this study suggests that a new HPV 16-positive test in a clinical setting may not indicate a new infection
The majority (approximately 90%) of newly acquired HPV infections become undetectable within 1–2 years, a phenomenon routinely described as “viral clearance,” but which may also represent immune control below detectable levels or viral latency (3):
- detectable immune response is generated approximately 60% of the time
- a minority of HPV infections are persistently detected beyond 12 months
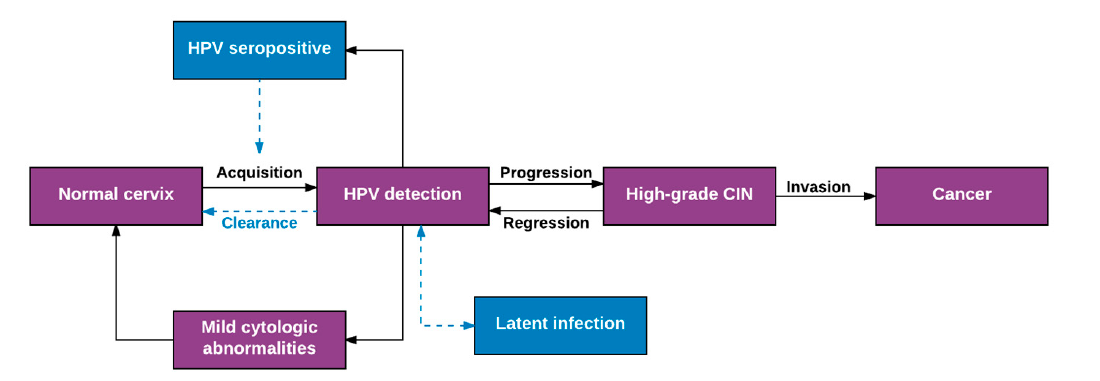
Schematic model of the population-level natural history of human papillomavirus infection and cervical cancer has been developed (3).
Purple boxes indicate well-accepted natural history model parameters; blue boxes represent uncertainties.
Gravitt et al have proposed an "Expanded View of HPV Natural History"
- the limitations of previous figure is that based on our understanding of the population-level natural history of HPV over the course of 5-10 years (the typical duration of prospective natural history studies)
- because of the practical limitations prohibiting longer duration studies, extrapolating this population-level model to the within-woman natural history of HPV infections over an entire life
- in most applications of HPV “incidence and clearance” estimates derived from this model, two critical assumptions prevail:
- (1) new HPV detection reflects recent acquisition either as a new infection or a re-infection; and
- (2) loss of HPV detection reflects viral clearance, or eradication
- model suggests that each HPV infection may follow a number of non-linear, non-mutually exclusive pathways over a woman’s life span. Specifically, new HPV detection can result not only from a recent sexual acquisition or re-infection, but also from recurrent detection of a controlled or latent infection, auto-inoculation from other epithelial sites (e.g., anus), or transient deposition of viral nucleic acid from a recent sex act. Similarly, loss of HPV detection (aka clearance) may reflect viral eradication with or without acquired immunity against re-infection or viral control below limits of detection (aka viral latency)
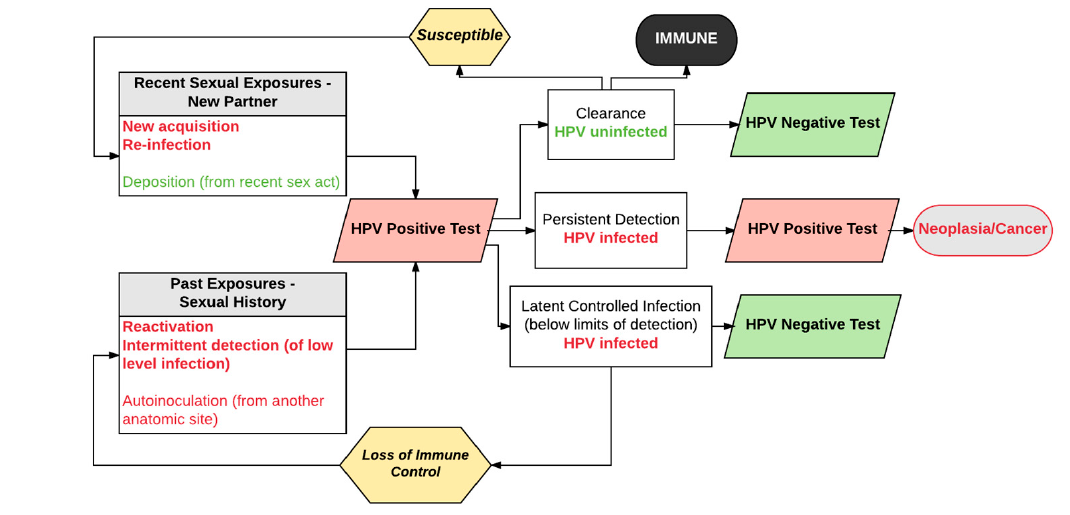
Schematic model of individual-level natural history of female genital HPV infection across the life span. The model assumes two pathways to type-specific HPV positivity after an HPV-negative test result—new acquisition or reinfection due to current sexual activity, or reactivation/recurrent detection of controlled, latent HPV infection. Red boxes indicate positive HPV molecular test results and green boxes indicate negative HPV molecular test results. Colored fonts represent the true underlying infectious status independent of concurrent molecular test results from exfoliated samples; red = HPV infection, green = HPV uninfected.
Reference:
- Brown BR, Weaver B. Human Papillomavirus in Older Women: New Infection or Reactivation?Journal of Infectious Diseases 2013;207:211–2
- Ermel A et al. Redetection of human papillomavirus type 16 infections of the cervix in mid-adult life. Papillomavirus Res. 2018 Jun;5:75-79
- Gravitt PE, Winer RL. Natural History of HPV Infection across the Lifespan: Role of Viral Latency. Viruses 2017 Oct; 9(10): 267.