management
Last edited 07/2021 and last reviewed 10/2022
Diagnosis:
- lesions can be swabbed and samples sent for culture
- NICE (1) do not suggest mandatory initial swabbing of lesions but note:
- if a skin swab has been sent for microbiological testing:
- review the choice of antibiotic when results are available and
- change the antibiotic according to results if symptoms are not improving, using a narrow-spectrum antibiotic if possible
Topical treatment:
- topical fusidic acid or mupirocin
- there is evidence that topical antibiotics may be slightly more effective than oral antibiotics for patients with limited non-bullous impetigo (2). Disinfecting treatments are not effective (2)
- topical antibiotic therapy is indicated in localized
cases without complications (3)
- topical mupirocin is a very effective treatment option
- topical fusidic acid cream an effective treatment for impetigo with very few side-effects, equally effective, in fact, as mupirocin.
Systemic treatment - if widespread
- systemic antimicrobials are the treatment of choice for widespread infections and infections complicated by systemic symptoms (3)
- recommended oral antibiotic choices are flucloxacillin or erythromycin, or a cephalosporin such as cefalexin or cefradine (4)
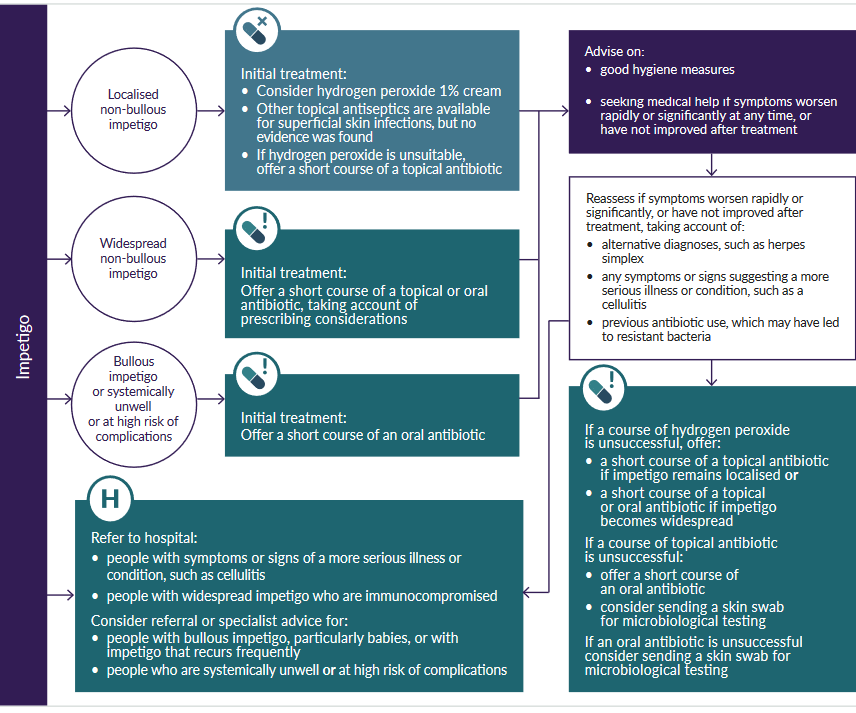
NICE suggest an algorithm for treatment based on features of the impetigo presenting to the clinician (1):
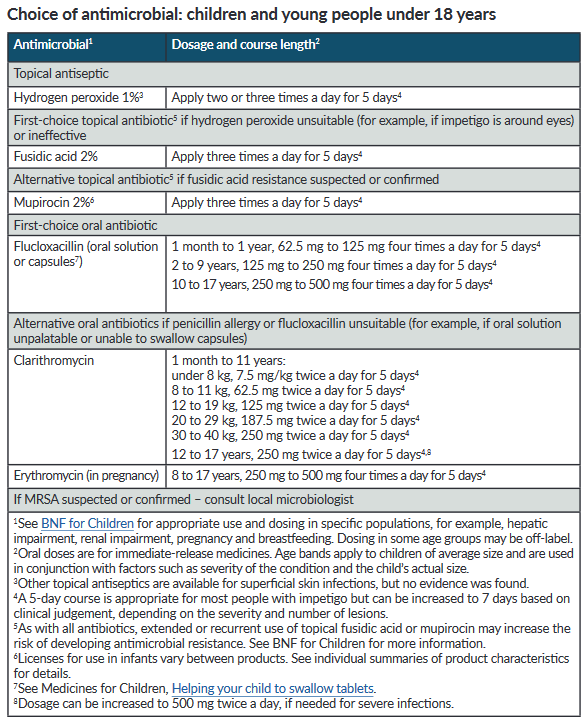
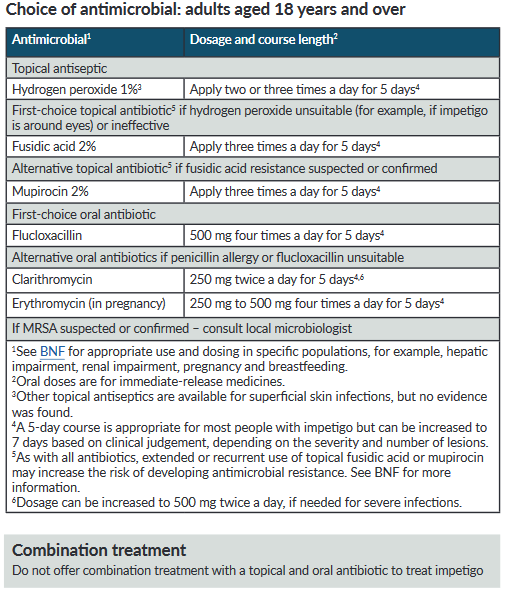
Antibiotic treatments have been suggested by NICE (1):
Patient eduction:
- good handwashing techniques
- avoid scratching - cutting finger-nails may be useful
Notes:
- previously been stated that topical treatment for 7 days is generally adequate for limited disease - the maximum duration of topical treatment is 10 days (4)
- if using systemic treatment and streptococcal infection is suspected then add phenoxymethylpenicillin to flucloxacillin (co-amoxiclav is an alternative to using phenoxymethylpenicillin and flucloxacillin together)
Reference:
- NICE (February 2020).Impetigo: antimicrobial prescribing
- Koning S etl al (2004). Interventions for impetigo. Cochrane Database Syst Rev 2004; (2)CD003261.
- Brown J et al. Impetigo: an update. Int J Dermatol. 2003 Apr;42(4):251-5
- Prescriber (2004); 15 (13): 35-40.
- Public Health England (June 2021). Managing common infections: guidance for primary care