systemic hypertension
Last edited 05/2021 and last reviewed 10/2023
Hypertension is high systemic arterial blood pressure. NICE define hypertension as persistent raised blood pressure 140/90 mmHg or higher (1).
Screening of the population for hypertension should be a priority because the condition is common, asymptomatic and has devastating complications.
- it has a strong association with cardiovascular diseases (CVD) and has become the leading risk factor for premature death in the world. High blood pressure has been attributed to
- 58% of haemorrhagic stroke
- 50% of ischaemic stroke
- 55% of ischaemic heart disease
- 58% of other cardiovascular diseases - including rheumatic and hypertensive heart disease, cardiomyopathy, rhythm or conduction disorders, aortic aneurysms, peripheral vascular disease and other cardiovascular diseases (2)
Blood pressure is normally distributed in the population and there is no natural cut-off point above which 'hypertension' definitively exists and below which it does not
- risk associated with increasing blood pressure is continuous, with each 2 mmHg rise in systolic blood pressure associated with a 7% increased risk of mortality from ischaemic heart disease and a 10% increased risk of mortality from stroke
- diastolic pressure is more commonly elevated in people younger than 50. With ageing, systolic hypertension becomes a more significant problem, as a result of progressive stiffening and loss of compliance of larger arteries
- at least one quarter of adults (and more than half of those older than 60) have high blood pressure
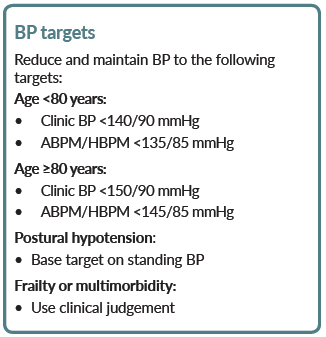
Blood pressure targets (1):
ABPM = ambulatory blood pressure monitoring
HBPM = home blood pressure monitoring
- if CKD and hypertension
- in people with CKD aim to keep the systolic blood pressure below 140 mmHg (target range 120-139 mmHg) and the diastolic blood pressure below 90 mmHg
- in people with CKD and diabetes, and also in people with an ACR of 70 mg/mmol or more, aim to keep the systolic blood pressure below 130 mmHg (target range 120-129 mmHg) and the diastolic blood pressure below 80 mmHg.
Assessment should also consider other risk factors for cardiovascular disease and stroke.
How effective is blood pressure lowering in reducing risk of cardiovascular events?
- in a large-scale analysis of randomised trials (4)
- a 5 mm Hg reduction of systolic blood pressure reduced the risk of major cardiovascular events (defined as a composite of fatal and non-fatal stroke, fatal or non-fatal myocardial infarction or ischaemic heart disease, or heart failure causing death or requiring admission to hospital) by about 10%, irrespective of previous diagnoses of cardiovascular disease, and even at normal or high-normal blood pressure values
- hazard ratios (HR) associated with a reduction of systolic blood pressure by 5 mm Hg for a major cardiovascular event
- in participants without previous cardiovascular disease was 0.91, 95% CI 0.89-0.94
- in partipants with previous cardiovascular disease was 0.89, 0.86-0.92
- findings suggest that a fixed degree of pharmacological blood pressure lowering is similarly effective for primary and secondary prevention of major cardiovascular disease, even at blood pressure levels currently not considered for treatment
- a 5 mm Hg reduction of systolic blood pressure reduced the risk of major cardiovascular events (defined as a composite of fatal and non-fatal stroke, fatal or non-fatal myocardial infarction or ischaemic heart disease, or heart failure causing death or requiring admission to hospital) by about 10%, irrespective of previous diagnoses of cardiovascular disease, and even at normal or high-normal blood pressure values
Notes:
- the diagnosis of hypertension should not be made on the basis of a single elevated reading. In many cases, a second blood pressure reading is lower, and often, a third lower still
- patients found to have malignant or accelerated phase hypertension should be referred to hospital as an emergency
- the majority of patients will have essential hypertension but it is nevertheless imperative to fully investigate for secondary causes
- a systematic review concluded (3):
- For the general population of persons with elevated blood pressure the small benefits of trying to achieve a lower blood pressure targetrather than a standard target (<=140/90 mm Hg) do not outweigh the harms
Reference:
- (1) NICE (August 2019). Clinical management of primary hypertension in adults
- (2) van Kleef ME, Spiering W. Hypertension: Overly important but under-controlled. Eur J Prev Cardiol. 2017;24(3_suppl):36-43.
- (3) Arguedas JA, Leiva V, Wright JM. Blood pressure targets in adults with hypertension. Cochrane Database of Systematic Reviews 2020, Issue 12. Art. No.: CD004349. DOI: 10.1002/14651858.CD004349.pub3
- (4) The Blood Pressure Lowering Treatment Trialists' Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021; 397: 1625-36.
types of systemic hypertension
classification of systemic hypertension
target blood pressure (BP ) levels
NICE guidance - hypertension management in type II diabetes
NICE guidance - management of hypertension in adults in primary care
referral criteria from primary care - hypertension
renal disease and hypertension
GPnotebook shortcut - lifestyle modifications to manage hypertension