psoriasis
Last edited 08/2019 and last reviewed 10/2023
Psoriasis is a common chronic skin disease characterised by cutaneous inflammation and epidermal hyperproliferation - lesions appear on any part of the skin, but particularly the scalp, sacral area, and over the extensor aspect of the knees and elbows
- the major manifestation of psoriasis is the chronic skin disease (although psoriatic joint disease is another major morbidity associated with psoriasis)
- psoriatic skin disease is characterised by cutaneous inflammation and epidermal
hyperproliferation (normally cells of the epidermal layer renew every 28 days,
but in psoriasis the regeneration occurs every 2 to 4 days) (1,2)
- lesions appear on any part of the skin, but particularly the scalp,
lumbosacral area and over the extensor aspect of the knees and elbows
(3).
- Characteristically, there are:
- well-defined, raised, erythematous and scaly lesions (3), which are "salmon pink" or "full rich red" in colour
- surface silvery scale which may be easily removed often leading to pin - point capillary bleeding (Auspitz sign) (4)
- they may or may not itch but this is not usually a prominent feature
- Characteristically, there are:
- lesions appear on any part of the skin, but particularly the scalp,
lumbosacral area and over the extensor aspect of the knees and elbows
(3).
- acute disease may manifest as inflammation and erythema while chronic lesions present as typical plaques (4). In most of the patients psoriasis presents in a chronic course with periods of remission (1).
- psoriasis is an emotionally and physically debilitating disease which is often underestimated by medical practioners (4)
A strong genetic predisposition can be seen in psoriasis. Around 8 genetic susceptibility loci (PSORS I-VIII) have been observed (1). Psoriasis susceptibility 1 (PSORS1) locus located on the 6th chromosome is considered to be the most important one and can be seen in up to 50% of psoriasis cases (3).
NICE suggest (4):
-
psoriasis is an inflammatory skin disease that typically follows a relapsing and remitting course - prevalence of psoriasis is estimated to be around 1.3-2.2% in the UK.
- is uncommon in children (0.71%) and the majority of cases occur before
35 years
- is associated with joint disease in a significant proportion of patients (reported in one study at 13.8%)
- plaque psoriasis is characterised by well-delineated red, scaly plaques
that vary in extent from a few patches to generalised involvement
- by far the most common form of the condition (about 90% of people with psoriasis)
- other types of psoriasis include guttate psoriasis and pustular (localised or generalised) forms
- distinctive nail changes occur in around 50% of all those affected and are more common in people with psoriatic arthritis
- several studies have also reported that people with psoriasis, particularly those with severe disease, may be at increased risk of cardiovascular disease, lymphoma and non-melanoma skin cancer
- therapeutics:
- first-line therapy describes traditional topical therapies (such as corticosteroids, vitamin D and vitamin D analogues, dithranol and tar preparations)
- second-line therapy includes the phototherapies (broad- or narrow-band ultraviolet B light and psoralen plus UVA light [PUVA]) and systemic non-biological agents such as ciclosporin, methotrexate and acitretin
- third-line therapy refers to systemic biological therapies such as the tumour necrosis factor antagonists adalimumab, etanercept and infliximab, and the monoclonal antibody ustekinumab that targets interleukin-12 (IL-12) and IL-23
A useful summary algorithm based on NICE guidance for management of psoriasis in adults has been produced (5). This is an excellent summary for management in primary care:
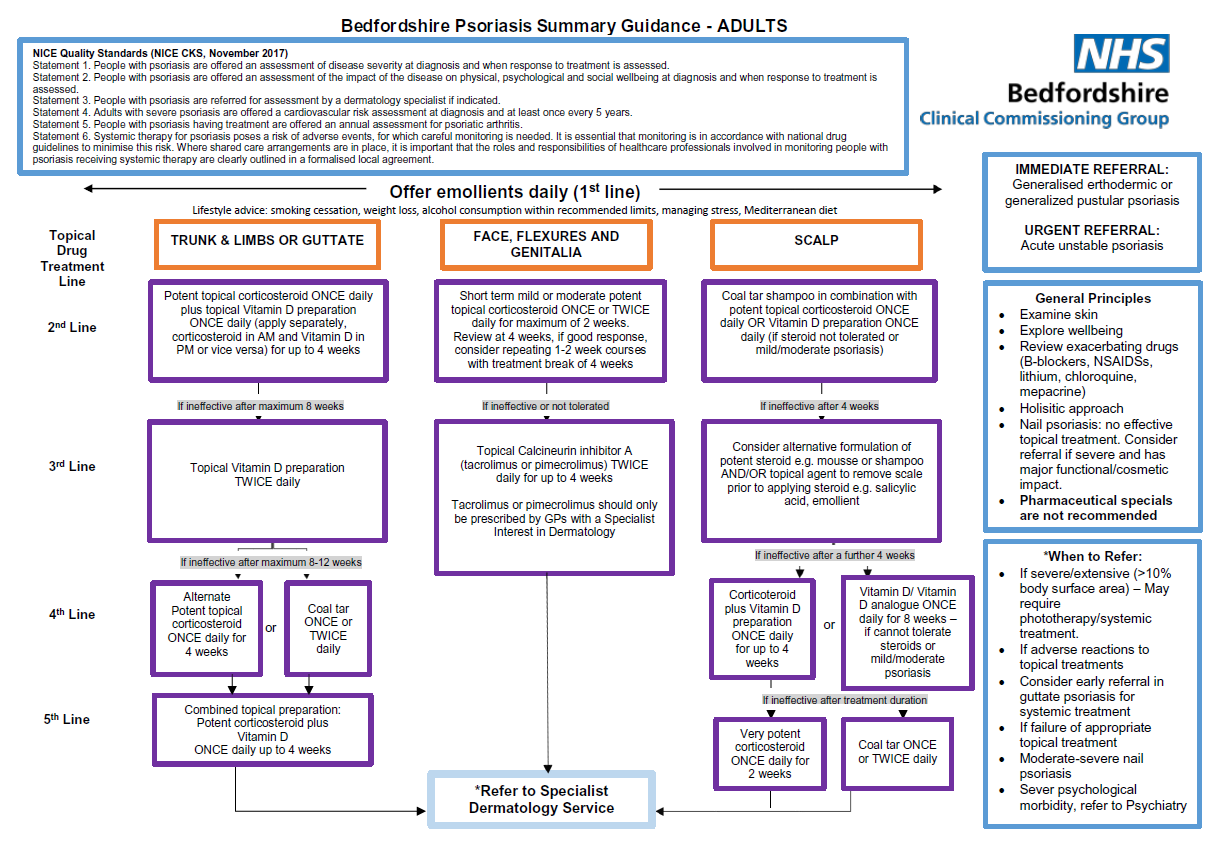

Notes (5):
| Mild steroid cream/ointment | Hydrocortisone 1% (cream/ ointment) |
Children: Any area up to twice a day Adults: Any area up to twice a day |
| Moderate steroid cream/ointment | Clobetasone butyrate 0.05% (cream/ointment) (Eumovate (R) |
Children: Up to twice a day. Face and flexures for severe flares max 3-5 days then reduce potency. Adults: all areas max twice a day |
| Moderate steroid cream/ointment | Betamethasone valerate 0.025% (cream/ointment) |
Children: Up to twice a day. Avoid face and flexures. Adults: all areas max twice a day |
| Potent* steroid cream/ointment | Betamethasone valerate 0.1% (cream/ointment) |
Children: Age <12 months: specialist initiation only Age>12 months: Short term use up to 14 days in areas like axilla and groin. Only if inadequate response to moderate steroid. Adults: body, limbs, feet and hands ONLY up to twice a day for max 7-14 days then reduce strength |
| Potent* steroid cream/ointment | Mometasone furoate 0.1% (cream/ointment) [Elocon (R)] |
Children: Only use if inadequate response to moderate steroid and when recommended by specialist in <12 months age. Use least amount possible once a day for no more than 5 days. Adults: Thin film of cream or ointment should be applied to affected areas once daily. If used on face, then max 5 days |
| Very potent* steroid cream/ointment | Clobetasol proprionate 0.05% (cream/ointment) |
Children: Never use without specialist advice. Adults: Never for face. Only for those unresponsive to potent steroids for a short course especially on hands or feet |
Key points when prescribing topical steroids:
- ointments should be used in the first instance if cosmetically acceptable. Creams contain more water and therefore may contain more preservatives - but they may be more cosmetically acceptable
- *there should be a four week gap between courses of potent/very potent steroid treatments
- refer to relevant product SPC (www.medicines.org.uk) for further information on side effects and excipients
Reference:
- 1. American Academy of Dermatology 2008. Guidelines of care for the management of psoriasis and psoriatic arthritis - Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics
- 2. American Academy of Dermatology. Psoriasis
- 3. Schon M.P, Boehncke W.H. Psoriasis. NEJM 2005;352:1899-1912.
- 4. Guillen S, Khachemaoune A. Photo quiz - Large, Silvery Plaques. AFP 2007;75(8)
- 4. NICE (September 2017). Psoriasis - the assessment and management of psoriasis
- 5. NHS Bedfordshire Clinical Commissioning Group. Bedfordshire Psoriasis Summary Guidance - adults (Accessed 21/8/2019).
diagnosis of psoriasis - general principles
general approaches to psoriasis treatment