management of unstable angina/non STEMI
Last edited 12/2020 and last reviewed 12/2020
Immediate referral to hospital:
- as soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin
and antithrombin therapy have been offered, formally assess individual risk
of future adverse cardiovascular events using an established risk scoring
system that predicts 6-month mortality (for example, Global Registry of Acute
Cardiac Events [GRACE])
- include in the formal risk assessment:
- a full clinical history (including age, previous myocardial infarction [MI] and previous percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG])
- a physical examination (including measurement of blood pressure and heart rate)
- resting 12-lead electrocardiography (ECG) (looking particularly for dynamic or unstable patterns that indicate myocardial ischaemia)
- blood tests (such as troponin I or T, creatinine, glucose and haemoglobin)
- include in the formal risk assessment:
NSTEMI and unstable angina – early management
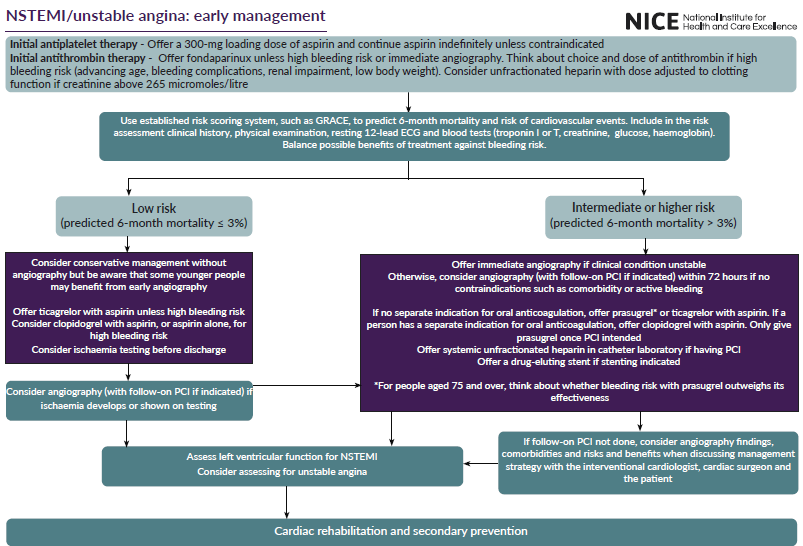
Initial drug therapy
- offer aspirin as soon as possible to all people with unstable angina or non-ST-segment elevation myocardial infarction (NSTEMI) and continue indefinitely unless contraindicated by bleeding risk or aspirin hypersensitivity
- offer people with unstable angina or NSTEMI a single loading dose of 300-mg aspirin as soon as possible unless there is clear evidence that they are allergic to it
- offer fondaparinux to people with unstable angina or NSTEMI who do not have a high bleeding risk, unless they are undergoing immediate coronary angiography
- consider unfractionated heparin, with dose adjustment guided by monitoring of clotting function, as an alternative to fondaparinux for people with unstable angina or NSTEMI and significant renal impairment (creatinine above 265 micromoles per litre)
- carefully consider the choice and dose of antithrombin for people with unstable angina or NSTEMI who have a high risk of bleeding associated with any of the following:
- advancing age
- known bleeding complications
- renal impairment
- low body weight
- do not offer dual antiplatelet therapy to people with chest pain before a diagnosis of unstable angina or NSTEMI is made
Risk assessment
- as soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin and antithrombin therapy have been offered, formally assess individual risk of future adverse cardiovascular events using an established risk scoring system that predicts 6-month mortality (for example, Global Registry of Acute Cardiac Events [GRACE])
- include in the formal risk assessment:
- a full clinical history (including age, previous myocardial infarction [MI] and previous PCI or coronary artery bypass grafting [CABG])
- a physical examination (including measurement of blood pressure and heart rate)
- a resting 12-lead ECG, looking particularly for dynamic or unstable patterns that indicate myocardial ischaemia
- blood tests (such as troponin I or T, creatinine, glucose and haemoglobin)
- record the results of the risk assessment in the person's care record
- use risk assessment to guide clinical management, and balance the benefit of a treatment against any risk of related adverse events in the light of this assessment
- use predicted 6-month mortality to categorise the risk of future adverse cardiovascular events as shown in table below
Table: Categorising risk of future adverse cardiovascular events
Risk of future adverse cardiovascular events
| Predicted 6-month mortality | Risk of future adverse cardiovascular events |
| 1.5% or below | Lowest |
| >1.5% to 3.0% | Low |
| >3.0% to 6.0% | Intermediate |
| >6.0% to 9.0% | High |
| over 9.0% | Highest |
Categories of risk are derived from the Myocardial Ischaemia National Audit Project (MINAP) database.
Coronary angiography with follow-on PCI
- offer immediate coronary angiography to people with unstable angina or NSTEMI if their clinical condition is unstable
- consider coronary angiography (with follow-on PCI if indicated) within 72 hours of first admission for people with unstable angina or NSTEMI who have an intermediate or higher risk of adverse cardiovascular events (predicted 6-month mortality above 3.0%) and no contraindications to angiography (such as active bleeding or comorbidity). See table 2 for information on the benefits and risks of early invasive treatment compared with conservative management
- consider coronary angiography (with follow-on PCI if indicated) for people with unstable angina or NSTEMI who are initially assessed to be at low risk of adverse cardiovascular events (predicted 6-month mortality 3.0% or less) if ischaemia is subsequently experienced or is demonstrated by ischaemia testing.
See table below for information on the benefits and risks of early invasive treatment compared with conservative management
- bBe aware that some younger people with low risk scores for mortality at 6 months may still be at high risk of adverse cardiovascular events and may benefit from early angiography
Benefits and risks of early invasive treatment (coronary angiography with PCI if needed) compared with conservative management for people with unstable angina or NSTEMI
| Benefits/risks/ other factors |
Coronary angiography and possible percutaneous coronary intervention (PCI) within 72 hours |
Conservative management with later coronary angiography if problems continue or develop |
| Benefits (advantages) | Reduced deaths from all causes at 6 to 12 months and at 2 years. Reduced deaths from heart problems at 1 and 2 years. Reduced incidence of myocardial infarction (MI) at 30 days, 6 to 12 months and 2 years. Reduced incidence of stroke at 1 year, particularly in people at high risk of future adverse events. Reduced readmission to hospital and difficult-to-treat angina in the medium term, particularly in people at high risk of future adverse events. Psychological benefits – people are not anxious about delaying angiography. |
Avoid the immediate risks of invasive treatment, including:
|
| Risks (disadvantages) | Increased risk of death during the first 4 months, particularly for people at low risk of future adverse events.
treatment leaves little time for shared decision making. |
Increased risk of MI after 6 months.
|
| Other factors | Recent advances in PCI might increase early benefit, particularly reducing bleeding.
|
- systemic unfractionated heparin should be offered in the cardiac catheter laboratory to people with unstable angina or NSTEMI who are undergoing PCI whether or not they have already received fondaparinux. In November 2020, this was an off-label use of unfractionated heparin. See NICE's information on prescribing medicines
- for people with unstable angina or NSTEMI who are having coronary angiography, offer:
- prasugrel or ticagrelor, as part of dual antiplatelet therapy with aspirin, if they have no separate indication for ongoing oral anticoagulation (if using prasugrel, only give it once coronary anatomy has been defined and PCI is intended, and use the maintenance dose in the prasugrel summary of product characteristics; for people aged 75 and over, think about whether the person's risk of bleeding with prasugrel outweighs its effectiveness)
- clopidogrel, as part of dual antiplatelet therapy with aspirin, if they have a separate indication for ongoing oral anticoagulation
- if stenting is indicated, offer a drug-eluting stent to people with unstable angina or NSTEMI undergoing revascularisation by PCI. [2020]
Management when PCI is not indicated
- consider conservative management without early coronary angiography for people with unstable angina or NSTEMI who have a low risk of adverse cardiovascular events (predicted 6-month mortality 3.0% or less)
- offer ticagrelor, as part of dual antiplatelet therapy with aspirin, to people with unstable angina or NSTEMI when PCI is not indicated, unless they have a high bleeding risk
- consider clopidogrel, as part of dual antiplatelet therapy with aspirin, or aspirin alone, for people with unstable angina or NSTEMI when PCI is not indicated, if they have a high bleeding risk
Reference:
- NICE (November 2020). Acute coronary syndromes.
NICE guidance - glycoprotein IIb/IIIa for unstable angina and NSTEMI
statin treatment in acute coronary syndrome
antithrombin therapy in unstable angina / NSTEMI
early versus invasive management for patients with unstable angina / NSTEMI
percutaneous coronary intervention versus coronary artery bypass grafting