treatment
Last edited 06/2019
Treatment of primary hyperparatyroidism can be
- parathyroid surgery
- in symptomatic disease - parathyroidectomy should be the treatment of first choice
- in asymptomatic disease - patients with the following criteria should be oferred surgery
- serum albumin-adjusted calcium - greater than 0.25 mmol/L above the upper limit
- calculated creatinine clearance - <60 mL/min.
- bone mineral density - T score of −2.5 or less at any site or previous fragility fracture (or both)
- age - younger than 50 years (1)
- before undrgoing surgery, an ultrasound scan of the neck and 99mTc-sestamibi scan to localise the parathyroid glands and any tumours should be carried out in all patients (2).
- complications of parathyroidectomy includes:
- voal cord paresis
- hypocalcaemia
- in total parathyroidectomy - requires lifelong oral calcium and vitamin D supplementation
- in partial parathyroidectomy or parathyroid adenomectomy - hypocalcaemia is usually transient (becomes norml when the remaining normal parathyroid tissue recovers)
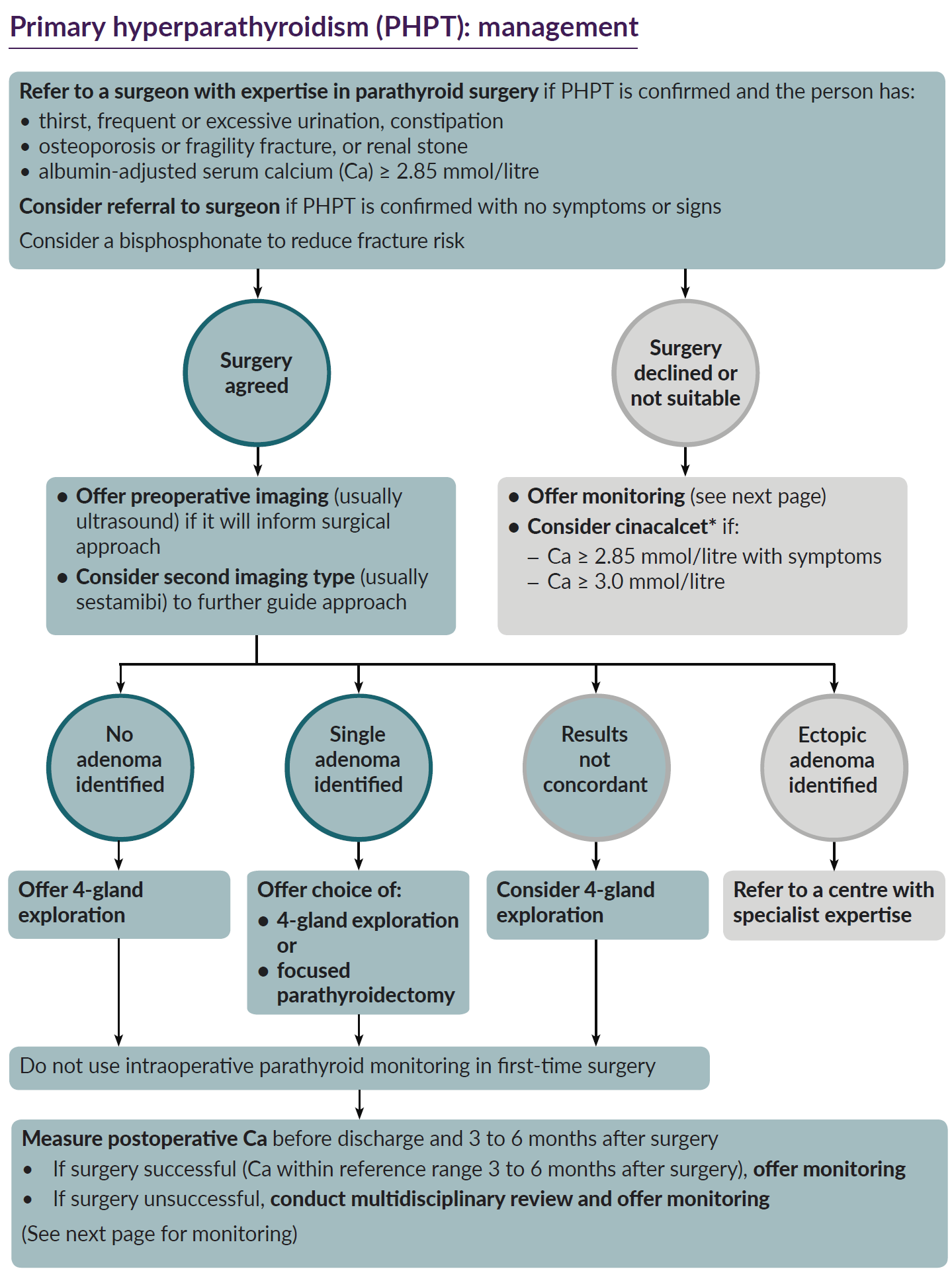
- NICE have suggested a schemata for management of primary hyperparathyroidism
(4)
-
- medical management
- considered in patients who do not meet the criteris for parathyroidectomy as well as those who are unwilling or unable to have surgery.
- monitoring guidance is included in linked item
- follow up is important since around 2-3 % of patients will develop new indications for surgery (1)
- patients should be advised about maintaining adequate hydration and avoiding thiazide diuretics and lithium
- NICE have suggested (4)
- non-surgical management
- calcimimetics
- cincalcet (*) should be considered for people with primary
hyperparathyroidism if surgery has been unsuccessful, is unsuitable
or has been declined, and if their albumin adjusted serum calcium
level is either:
- 2.85mmol/litre or above with symptoms of hypercalcaemia or
- 3.0 mmol/litre or above with or without symptoms of hypercalcaemia
- if initial albumin-adjusted serum calcium level is 2.85 mmol/ litre or above with symptoms of hypercalcaemia, base decisions on whether to continue treatment with cinacalcet on how well it reduces symptoms
- if initial albumin-adjusted serum calcium level is 3.0 mmol/litre or above, base decisions on whether to continue treatment with cinacalcet on how well it reduces either symptoms or albumin-adjusted serum calcium level
- cincalcet (*) should be considered for people with primary
hyperparathyroidism if surgery has been unsuccessful, is unsuitable
or has been declined, and if their albumin adjusted serum calcium
level is either:
- bisphosphonates
- bisphosphonates should be considered to reduce fracture risk for people with primary hyperparathyroidism and increased fracture risk
- do not offer bisphosphonates for chronic hypercalcaemia of primary hyperparathyroidism.
- calcimimetics
- non-surgical management
* At the time of publication (May 2019), cinacalcet did not have a UK marketing authorisation for use after unsuccessful surgery for primary hyperparathyroidism. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council's Prescribing guidance: prescribing unlicensed medicines for further information
Reference:
- (1) Pallan S, Rahman MO, Khan AA. Diagnosis and management of primary hyperparathyroidism. BMJ. 2012;344:e1013
- (2) Rogers A, Wass J. Clinical review:Hyperparatyroidism. GP online 2011
- (3) Cinacalcet treatment of primary hyperparathyroidism: biochemical and bone densitometric outcomes in a five-year study. J Clin Endocrinol Metab 2009; 94:4860-7.
- (4) NICE (May 2019). Primary Hyperparathyoridism.