acute coronary syndrome (ACS)
Last edited 12/2020 and last reviewed 12/2020
Acute coronary syndromes due to ischaemic heart disease remain a significant cause of morbidity and mortality
- in 2015, heart disease remained the leading cause of death in men and the second most common cause of death in women in England
- in 2015/16, more than 58,000 people were admitted to hospital in England with a heart attack. Although many more people now survive than in the past, there remains considerable scope to reduce their future risk of death, angina, heart failure and further heart attack
- acute coronary syndrome (ACS) encompasses previous terms such as non-Q wave myocardial infarction and unstable angina (1)
- ACS is defined as:
- 1. unstable angina (symptoms at rest with ECG changes)
- 2. Non STEMI (non ST elevation myocardial infarction) with at least
two of the following criteria
- symptoms at rest
- raised serum Troponin
- ECG changes
- 3. STEMI (ST elevation myocardial infarction) symptoms with ST elevation
on ECG
- acute coronary syndromes encompass a spectrum of unstable coronary artery
disease from unstable angina to transmural myocardial infarction
- all have a common aetiology in the formation of thrombus on an inflamed and complicated atheromatous plaque
- principles behind the presentation, investigation and management of these syndromes are similar with important distinctions depending on the category of acute coronary syndrome
Clinical presentation and immediate assessment
- patients with suspected acute coronary syndrome should be assessed immediately by an appropriate healthcare professional and a 12 lead electrocardiogram should be performed
- repeat 12 lead electrocardiograms should be performed if there is diagnostic uncertainty or a change in the clinical status of the patient, and at hospital discharge
- patients with persisting bundle branch block or ST segment change should be given a copy of their electrocardiogram to assist their future clinical management should they represent with a suspected acute coronary syndrome
Biochemical diagnosis
- in patients with suspected acute coronary syndrome, serum troponin concentration should be measured on arrival at hospital to guide appropriate management and treatment
- to establish a diagnosis in patients with an acute coronary syndrome, a serum troponin concentration should be measured 12 hours from the onset of symptoms
- to establish a diagnosis in patients with an acute coronary syndrome when symptom onset is uncertain, serum troponin concentration should be measured 12 hours from presentation
- when considering a diagnosis of ACS, serum troponin concentrations should not be interpreted in isolation but with regard to the clinical presentation of the patient
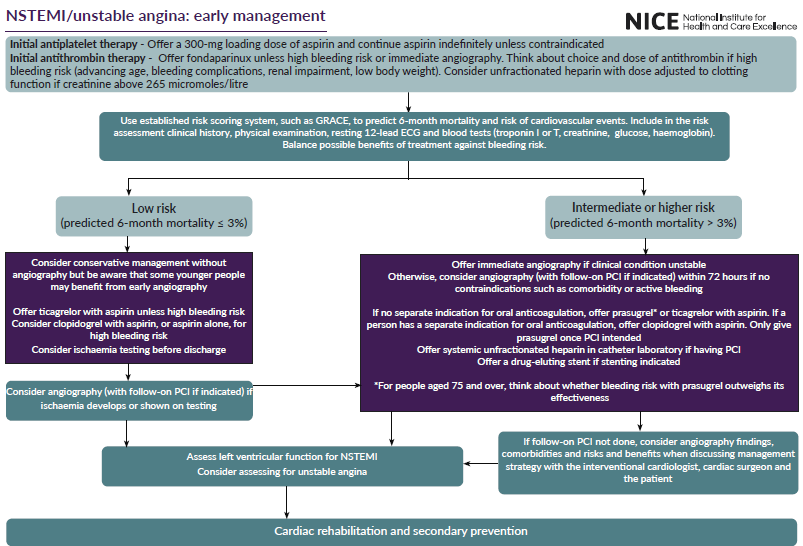
Management is guided based on whether STEMI or NSTEMI/unstable angina
If STEMI:

If NSTEMI/unstable angina:
A study investigating one-year mortality following diagnosis of acute coronary syndrome showed (3):
- mortality rate was 3.9% within one year of discharge
- independent mortality predictors identified (in order of predictive strength):
- age, lower ejection fraction, poorer EQ-5D quality of life, elevated serum creatinine, in-hospital cardiac complications, chronic obstructive pulmonary disease, elevated blood glucose, male gender, no PCI/CABG after NSTEMI, low hemoglobin, peripheral artery disease, on diuretics at discharge
A study investigating two-year mortality following diagnosis of acute coronary syndrome showed (3):
- mortality rate was 5.5% within two years of discharge
- independent mortality predictors identified were:
- age, low ejection fraction, no coronary revascularization/thrombolysis, elevated serum creatinine, poor EQ-5D score, low haemoglobin, previous cardiac or chronic obstructive pulmonary disease, elevated blood glucose, on diuretics or an aldosterone inhibitor at discharge, male sex, low educational level, in-hospital cardiac complications, low body mass index, ST-segment elevation myocardial infarction diagnosis, and Killip class
Data from a large Swedish registry including 108 315 post-MI patients with long-term follow-up revealed a cumulative rate of a cardiovascular composite endpoint (cardiovascular death, recurrent MI, and stroke) of 18.3% in the first year after MI, 9.0% in the subsequent year and 20.0% in the following 3 years (4)
Reference:
- NICE (2010). Unstable angina and NSTEMI -the early management of unstable angina and non-ST-segment-elevation myocardial infarction.
- NICE (November 2020). Acute coronary syndromes.
- Pocock S, Bueno H, Licour M, Medina J, Zhang L, Annemans L, Danchin N, Huo Y, Van de Werf F. Eur Heart J Acute Cardiovasc Care. 2015 Dec; 4(6):509-17. Epub 2014 Oct 9.
- Pocock SJ et al.Predicting two-year mortality from discharge after acute coronary syndrome: An internationally-based risk score.Eur Heart J Acute Cardiovasc Care. 2019 Dec; 8(8):727-737. Epub 2017 Aug 4.
- Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36:1163-1170
non-Q wave myocardial infarction
STEMI (ST elevation myocardial infarction)
non STEMI (ST elevation myocardial infarction)
acute coronary syndrome (ACS) and driving
immediate management of suspected acute coronary syndrome
assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin
assessment in hospital in patients with acute coronary syndrome
Killip classification of heart failure