diagnosis of asthma in adults and children
Last edited 11/2019
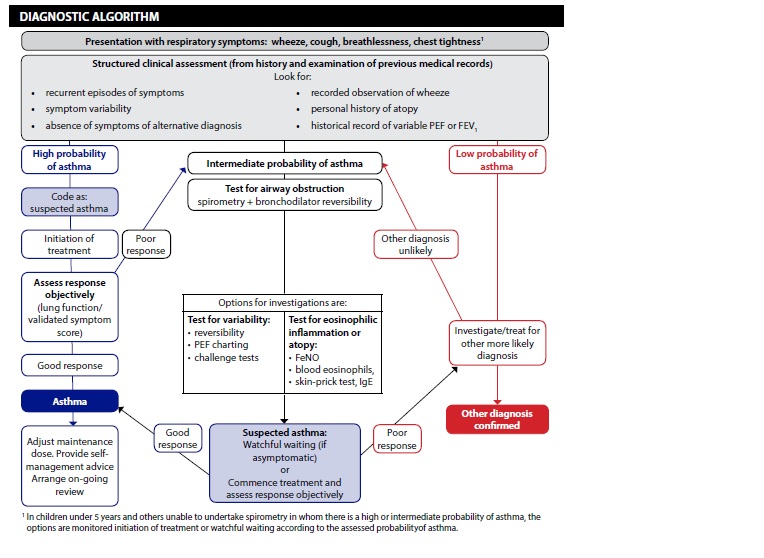
Diagnosis of asthma is based on the recognition of a characteristic pattern of symptoms and signs and the absence of an alternative explanation for them.
Diagnosis - initial structured assessment:
The predictive value of individual symptoms or signs is poor, and a structured clinical assessment including all information available from the history, examination and historical records should be undertaken.
Factors to consider in an initial structured clinical assessment include:
- Episodic symptoms
- more than one of the symptoms of wheeze, breathlessness, chest tightness
and cough occurring in episodes with periods of no (or minimal) symptoms
between episodes. Note that this excludes cough as an isolated symptom
in children. For example:
- a documented history of acute attacks of wheeze, triggered by viral
infection or allergen exposure with symptomatic and objective improvement
with time and/or treatment
- recurrent intermittent episodes of symptoms triggered by allergen
exposure as well as viral infections and exacerbated by exercise and
cold air, and emotion or laughter in children
- in adults, symptoms triggered by taking non-steroidal anti-inflammatory
medication or beta blockers
- a documented history of acute attacks of wheeze, triggered by viral
infection or allergen exposure with symptomatic and objective improvement
with time and/or treatment
- more than one of the symptoms of wheeze, breathlessness, chest tightness
and cough occurring in episodes with periods of no (or minimal) symptoms
between episodes. Note that this excludes cough as an isolated symptom
in children. For example:
- an historical record of significantly lower FEV1 or PEF during symptomatic
episodes compared with asymptomatic periods provides objective confirmation
of the obstructive nature of the episodic symptoms
- wheeze confirmed by a healthcare professional on auscultation
- It is important to distinguish wheezing from other respiratory noises,
such as stridor or rattly breathing. Repeatedly normal examination of
chest when symptomatic reduces the probability of asthma
- It is important to distinguish wheezing from other respiratory noises,
such as stridor or rattly breathing. Repeatedly normal examination of
chest when symptomatic reduces the probability of asthma
- evidence of diurnal variability
- symptoms which are worse at night or in the early morning
- symptoms which are worse at night or in the early morning
- atopic history
- personal history of an atopic disorder (ie eczema or allergic rhinitis)
or a family history of asthma and/or atopic disorders, potentially corroborated
by a previous record of raised allergen-specific IgE levels, positive
skin-prick tests to aeroallergens or blood eosinophilia
- personal history of an atopic disorder (ie eczema or allergic rhinitis)
or a family history of asthma and/or atopic disorders, potentially corroborated
by a previous record of raised allergen-specific IgE levels, positive
skin-prick tests to aeroallergens or blood eosinophilia
- Absence of symptoms, signs or clinical history to suggest alternative diagnoses (including but not limited to COPD, dysfunctional breathing, obesity).
Assess probablity of asthma based on initial clinical assessment:
High Probability:
Adults and children with a typical clinical assessment including recurrent episodes of symptoms (attacks), wheeze heard by a healthcare professional, historical record of variable airflow obstruction and a positive history of atopy and without any features to suggest an alternative diagnosis have a high probability of asthma.
In patients with a high probability of asthma:
- record the patient as likely to have asthma and commence a carefully monitored
initiation of treatment (typically 6 weeks of inhaled corticosteroids)
- assess the patient's status with a validated symptom questionnaire ideally
corroborated by lung function tests (FEV1 at clinic visits or by domiciliary
serial peak flows to capture times with/without symptoms)
- with a good symptomatic and objective response to treatment, confirm the
diagnosis of asthma and record the basis on which the diagnosis was made
- if response is poor or equivocal, check inhaler technique and adherence, arrange further tests and consider alternative diagnoses
Low Probability:
Adults and children who do not have any of the typical features on initial structured clinical assessment or who have symptoms suggestive of an alternative diagnosis have a low probability of asthma.
- If there is a low probability of asthma and/or an alternative diagnosis
is more likely, investigate for the alternative diagnosis reconsidering asthma
if the clinical picture changes or an alternative diagnosis is not confirmed
- If reconsidering asthma, undertake or refer for further tests to investigate for a diagnosis of asthma.
Intermediate Probability:
Adults and children who have some, but not all, of the typical features of asthma on an initial structured clinical assessment or who do not respond well to a monitored initiation of treatment have an intermediate probability of asthma
Spirometry, with bronchodilator reversibility as appropriate, is the preferred initial test for investigating intermediate probability of asthma in adults, and in children old enough to produce reliable results on testing.
- In adults and children with an intermediate probability of asthma and airways
obstruction identified through spirometry, undertake reversibility tests and/or
a monitored initiation of treatment assessing the response to treatment by
repeating lung function tests and objective measures of asthma control
- In adults and children with an intermediate probability of asthma and normal
spirometry results, undertake challenge tests and/or measurement of FeNO to
identify eosinophilic inflammation
- In children with an intermediate probability of asthma who cannot
perform spirometry:
- consider watchful waiting if the child is asymptomatic
- offer a carefully monitored trial of treatment if the child is symptomatic.
Check for possible occupational asthma by asking employed people with suspected new-onset asthma, or established asthma that is poorly controlled:
- are symptoms better on days away from work?
- are symptoms better when on holiday?
Make sure all answers are recorded for later review (2).
Reference: