management of acute sore throat in primary care
Last edited 03/2020
- establish the reason for the consultation
- establish the duration of the illness - infections usually resolve within five days
- review other risk factors
- consider aetiology of sore throat - most frequently look for features suggesting:
- an infective cause
- an indication for antibiotics
- analgesia (1):
- paracetamol and NSAIDs have good evidence of action in adults and are safe in the majority of cases
- paracetamol and NSAIDs are safe, in most cases, in paediatric patients, but codeine should be used with caution
- anaesthetic mouth washes have some evidence of benefit and should be considered for symptomatic relief
- soluble paracetamol held in the mouth and then swallowed eases the discomfort (2)
Summary of Public Health England (PHE) guidance regarding antibiotic treatment of sore throat (3)
- in general, avoid antibiotics as 90% resolve in 7 days without, and pain only reduced by 16 hours
- if Centor score 3 or 4: (Lymphadenopathy; No Cough; Fever; Tonsillar Exudate) - consider 2 or 3-day delayed or immediate antibiotics or rapid antigen test
- antibiotics to prevent Quinsy number needed to treat (NNT) >4000
- antibiotics to prevent Otitis media NNT 200
- 10d penicillin lower relapse vs 7d in RCT in <18yrs
NICE suggest (4):
- base use of antibiotics on the FEVERpain or Centor Criteria scores

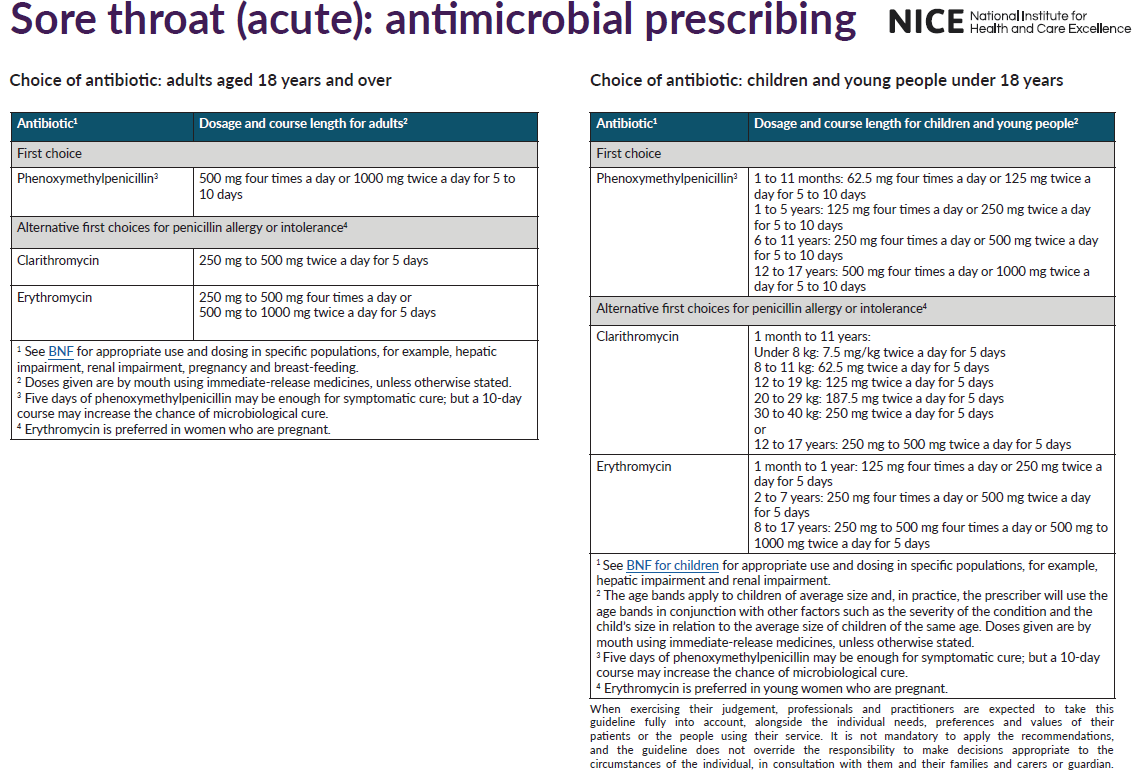
Antibiotics appropriate for management of sore throat (2):
Reference:
- Bird JH et al. Controversies in the management of acute tonsillitis: an evidence-based review.Clin Otalaryngol. 2014 Dec;39(6):368-74
- Prescriber (2000);11 (23): 83-87.
- Public Health England (October 2014). Management of infection guidance for primary care for consultation and local adaptation
- NICE (January 2018). Sore throat (acute): antimicrobial prescribing.
features suggesting an infective cause for a sore throat
delayed or back up antibiotic prescription in sore throat
Centor criteria to aid diagnosis of Group A beta-haemolytic streptococcus