hepatitis B serology summary
Last reviewed 01/2018
| Tests | Results | Interpretation |
|
HBsAg Anti-HBc Anti-HBs |
Negative Negative Negative |
Naïve, susceptible |
|
HBsAg Anti-HBc Anti-HBs |
Negative Positive Positive |
Immune due to natural infection |
|
HBsAg Anti-HBc Anti-HBs |
Negative Negative Positive |
Immune due to Hepatitis B vaccination |
|
HBsAg Anti-HBc IgM Anti-HBc Anti-HBs |
Positive Positive Positive Negative |
Acutely infected |
|
HBsAg Anti-HBc IgM Anti-HBc Anti-HBs |
Positive Positive Positive or Negative Negative |
Chronically infected |
|
HBsAg Anti-HBc Anti-HBs |
Negative Positive Negative |
|
Source: Dr John Wong, Consultant Gastroenterologist, University Hospitals Coventry and Warwickshire (May 2008).
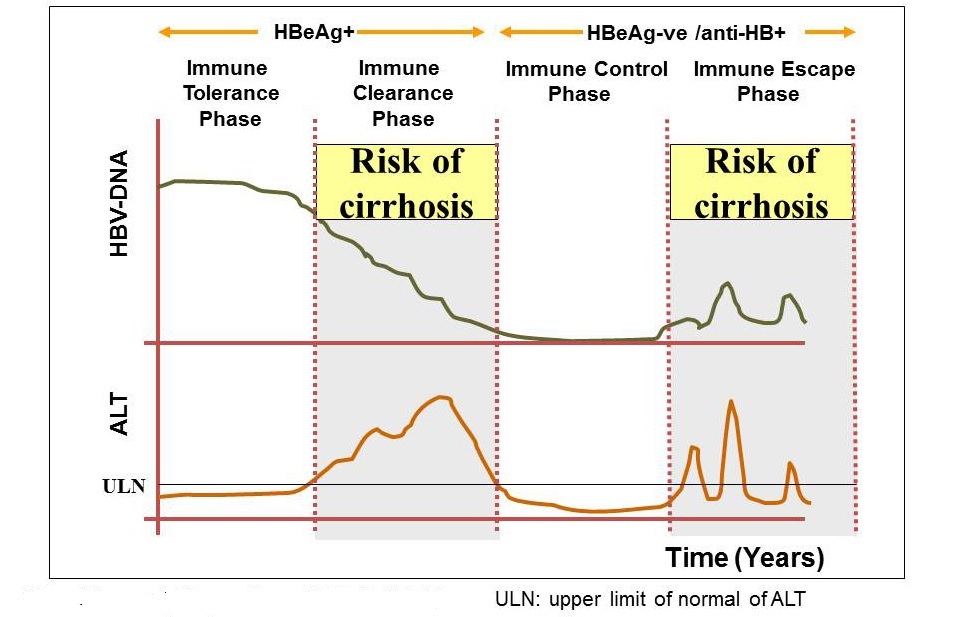
Phases of Hepatitis B infection - relates HbeAg and HBV DNA levels
- immune-tolerance phase
- the immune-tolerance phase is seen in HBeAg-positive disease and is characterised by high levels of HBV replication with normal ALT levels and limited liver necroinflammation
- because there is minimal immune response to the virus it is unusual for spontaneous HBeAg loss to occur
- this phase is commonly seen in children
- immune-clearance phase
- followed by an immune-clearance or immune-reactive phase in which
the immune system recognises and starts to clear the virus
- ALT levels are typically elevated or fluctuating, and there is a higher risk of liver fibrosis
- tends to be the initial phase in people infected with HBV as
adults
- lasts from weeks to years and ends with HBeAg seroconversion
- lasts from weeks to years and ends with HBeAg seroconversion
- followed by an immune-clearance or immune-reactive phase in which
the immune system recognises and starts to clear the virus
- immune-control phase
- with the loss of HBeAg the person may enter an immune-control phase with very low or undetectable HBV DNA levels, normal ALT and minimal fibrosis progression
- anti-HBe positive
- immune-escape phase
- however, some people may experience rising HBV DNA levels despite
HBeAg negativity. This is caused by virions that do not express HBeAg
because of genetic mutations
- this immune-escape phase can lead to active necroinflammation and progression of fibrosis
- anti-HBe positive
- however, some people may experience rising HBV DNA levels despite
HBeAg negativity. This is caused by virions that do not express HBeAg
because of genetic mutations
Notes:
-
HBeAg seroconversion
- HBeAg seroconversion occurs when people infected with the HBeAg-positive
form of the virus develop antibodies against the 'e' antigen.
- the seroconverted disease state is referred to as the 'inactive
HBV carrier state' when HBeAg has been cleared, anti-HBe is present
and HBV DNA is undetectable or less than 2000 IU/ml. Once seroconversion
has taken place, most people remain in the inactive HBV carrier state
(the immune-control phase)
- however, increasing HBV DNA and recurrent hepatitis after seroconversion indicate the emergence of the HBeAgnegative strain of the virus (the immune-escape phase). people may experience rising HBV DNA levels despite HBeAg negativity. This is caused by virions that do not express HBeAg because of genetic mutations. This immune-escape phase can lead to active necroinflammation and progression of fibrosis
- the seroconverted disease state is referred to as the 'inactive
HBV carrier state' when HBeAg has been cleared, anti-HBe is present
and HBV DNA is undetectable or less than 2000 IU/ml. Once seroconversion
has taken place, most people remain in the inactive HBV carrier state
(the immune-control phase)
- HBeAg seroconversion occurs when people infected with the HBeAg-positive
form of the virus develop antibodies against the 'e' antigen.
-
a form of the virus that does not cause infected cells to secrete HBeAg has been discovered (sometimes called the 'precore mutant' strain)
- people can be infected with the so-called HBeAg-negative form of the virus from the beginning, or the viral mutation can emerge later in the course of infection in people initially infected with the HBeAg-positive form of the virus
- prevalence of HBeAg-negative hepatitis varies geographically; it is more common in Asia and the Mediterranean region than in Northern Europe
Reference: