angina pectoris
Last edited 11/2019
Angina is described as a clinical syndrome of chest pain or pressure that accompanies periods of myocardial ischaemia; it is usually the manifestation of coronary artery disease. It is usually aggravated by activities which increases myocardial demand for oxygen e.g. - exercise and emotional stress (1). The name is derived from the Greek 'agkone' which means strangling.
The mechanism of pain sensation is uncertain: the metabolic products of ischamia stimulate pain fibres which pass to the sympathetic ganglia between C7 and T4. The pain is then referred to the corresponding peripheral dermatomes.
The chest pain is usually a central, constricting discomfort which may radiate to the jaw, neck, or one or both arms and may be associated with shortness of breath.
The Health Survey for England (2006) reported that around 8% of men and 3% of women aged between 55 and 64 years currently have or have had angina (2)
- figures for men and women aged between 65 and 74 years are around 14% and 8% respectively. It is estimated that almost 2 million people in England currently have or have had angina
SIGN state that despite a steep decline in mortality from coronary artery disease (CAD) in Scotland over the last 20 years, CAD remains one of the leading causes of death in Scotland, responsible for 7,154 deaths in 2015 (1)
- estimated that 18% of men aged 65-74 and 32% of men aged 75 and over are living with ischaemic heart disease ((IHD) heart attack or angina); the prevalence in women in these age groups is substantially lower at 9% and 20% respectively
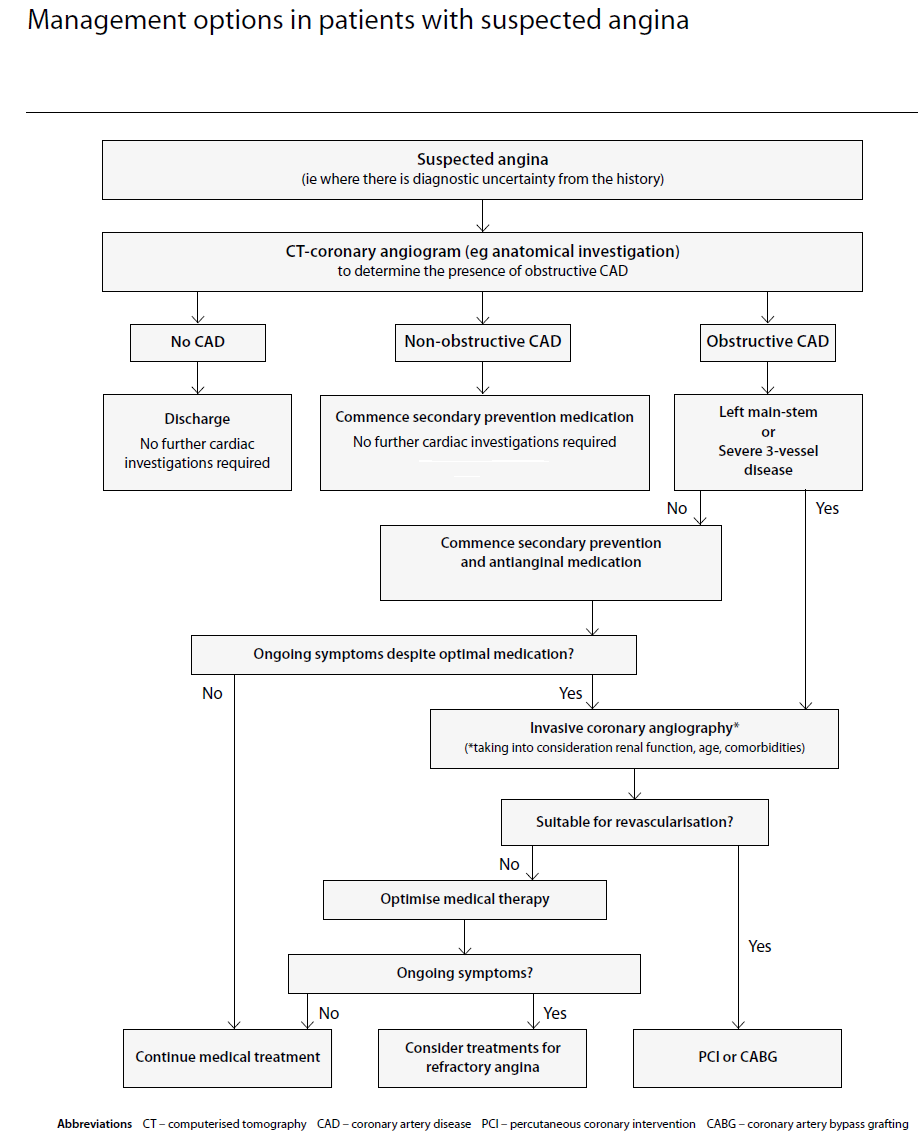
SIGN have outlined the management options in suspected angina (1):
- computerised tomography-coronary angiography should be considered for the initial investigation of patients with chest pain in whom the diagnosis of stable angina is suspected but not clear from history alone
- in patients with suspected stable angina, the exercise tolerance test should not be used routinely as a first-line diagnostic tool
- coronary angiography should be considered after non-invasive testing where patients are identified to be at high risk or where a diagnosis remains unclear
Reference:
- 1. SIGN (April 2018). Management of Stable Angina.
- 2. NICE (August 2016). Stable angina.
assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin
investigation of possible angina