management of vitamin D deficiency in adults
Last edited 12/2018
Seek expert advice or consult local guidelines.
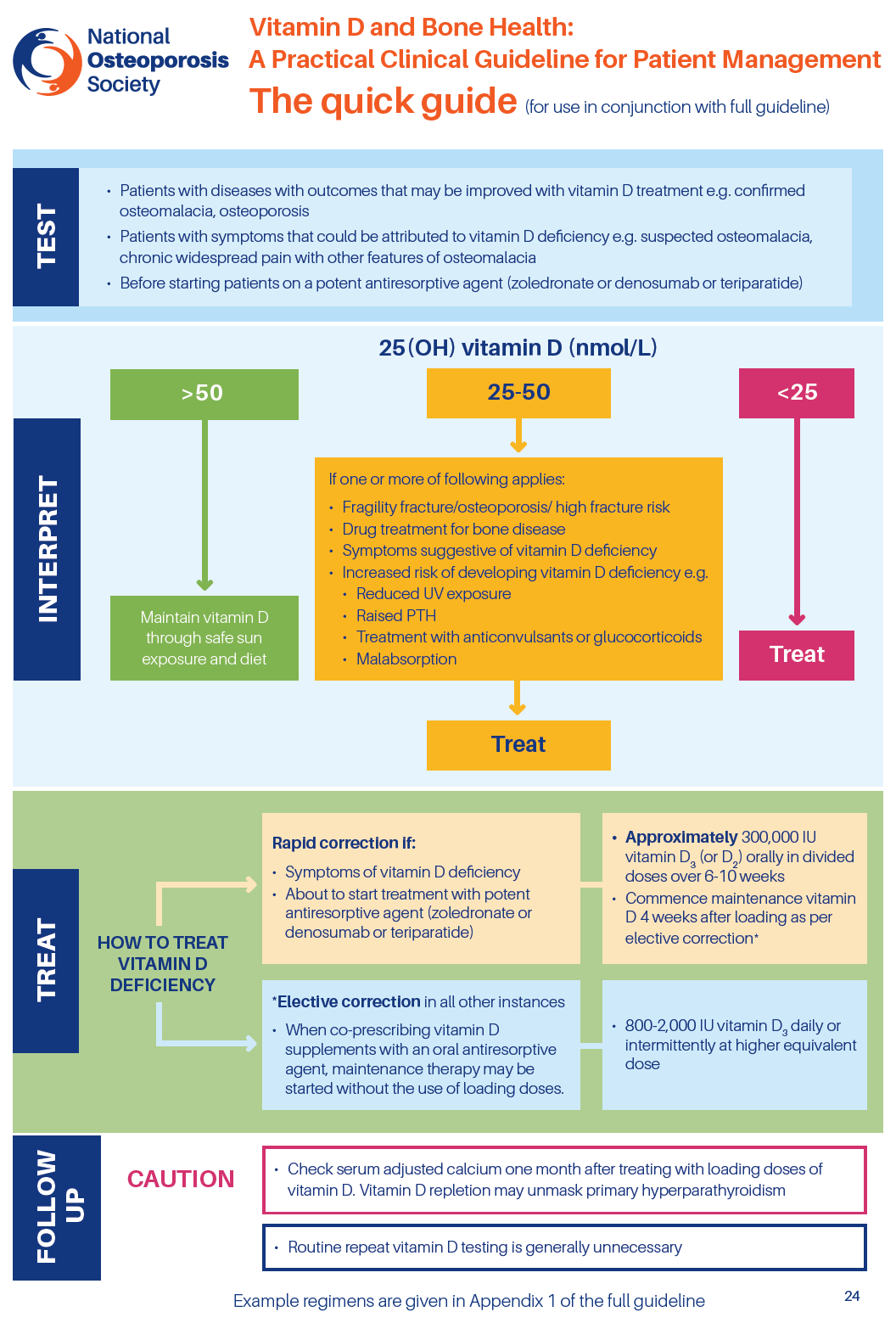
- serum vitamin D measurement is recommended for (1):
- plasma 25(OH)D measurement is recommended for:
- patients with musculoskeletal symptoms that could be attributed to vitamin D deficiency
- patients suspected of having bone diseases that may be improved with vitamin D treatment
- patients with bone diseases, prior to specific treatment where correcting
vitamin D deficiency may be necessary
- plasma 25(OH)D measurement is recommended for:
- routine monitoring of plasma 25(OH)D is generally unnecessary but may be
appropriate in patients with symptomatic vitamin D deficiency or malabsorption
and where poor compliance with medication is suspected (1)
- in most cases routine vitamin D testing is unnecessary in patients with
osteoporosis or fragility fracture, who may be co-prescribed vitamin D supplementation
with an oral antiresorptive treatment (1)
- where rapid correction of vitamin D deficiency is required, such as in patients
with symptomatic disease or about to start treatment with a potent antiresorptive
agent (zoledronate or denosumab or teriparatide), the recommended treatment
regimen is based on fixed loading doses followed by regular maintenance therapy
(1):
- a loading regimen to provide a total of approximately 300,000 IU vitamin D, given either as separate weekly or daily doses over six to ten weeks
- maintenance therapy comprising vitamin D in doses equivalent to 800-2,000
IU daily (occasionally up to a maximum of 4,000 IU daily), given either
daily or intermittently at higher doses
- where correction of vitamin D deficiency is less urgent and when co-prescribing
vitamin D supplements with an oral antiresorptive agent, maintenance therapy
may be started without the use of loading dose (1)
Treatment of vitamin D deficiency in adults (1):
- the following adult vitamin D thresholds are adopted by UK practitioners
in respect to bone health:
- serum vitamin D (serum 25OHD) < 30 nmol/L is deficient serum
- 25OHD of 30-50 nmol/L may be inadequate in some people serum
- 25OHD > 50 nmol/L is sufficient for almost the whole population
- treatment thresholds (1):
- Serum 25OHD < 30 nmol/L: treatment recommended
- Serum 25OHD 30-50 nmol/L: treatment is advised in patients with
the following:
- fragility fracture, documented osteoporosis or high fracture risk
- treatment with antiresorptive medication for bone disease
- symptoms suggestive of vitamin D deficiency
- increased risk of developing vitamin D deficiency in the future because of reduced exposure to sunlight, religious/cultural dress code, dark skin, etc.
- raised PTH
- medication with antiepileptic drugs or oral glucocorticoids
- conditions associated with malabsorption
- serum 25OHD > 50 nmol/L: provide reassurance and give advice
on maintaining adequate vitamin D levels through safe sunlight exposure
and diet
- Serum 25OHD < 30 nmol/L: treatment recommended
- oral vitamin D3 (colecalciferol) is the treatment of choice in vitamin
D deficiency (1)
- where rapid correction of vitamin D deficiency is required, such as in patients
with symptomatic disease or about to start treatment with a potent antiresorptive
agent (zoledronate or denosumab), the recommended treatment regimen is based
on fixed loading doses followed by regular maintenance therapy:
- a loading regimen to provide a total of approximately 300,000 IU vitamin D, given either as separate weekly or daily doses over 6 to 10 weeks
- maintenance therapy comprising vitamin D in doses equivalent to 800-2000
IU daily (occasionally up to 4,000 IU daily), given either daily or intermittently
at higher doses
- 1) Loading regimens for treatment of deficiency up to a total of
approximately 300,000 IU given either as weekly or daily split doses.
The exact regimen will depend on the local availability of vitamin D preparations
but will include:
- 50,000 IU capsules, one given weekly for 6 weeks (300,000 IU)
- 20,000 IU capsules, two given weekly for 7 weeks (280,000 IU)
- 800 IU capsules, five a day given for 10 weeks (280,000 IU)
- the following should be borne in mind:
- supplements should be taken with food to aid absorption
- calcium/vitamin D combinations should not be used as sources of vitamin D for the above regimens, given the resulting high dosing of calcium
- 2) Maintenance regimens may be considered 1 month after loading with doses equivalent to 800 to 2000 IU daily (occasionally up to 4,000 IU daily), given either daily or intermittently at a higher equivalent dose.
Monitoring:
all patients receiving pharmacological doses of vitamin D should have the plasma-calcium concentration checked at intervals (initially weekly) and whenever nausea or vomiting are present (3)
- NOS recommend checking adjusted serum calcium 1 month after completing the loading regimen or after starting vitamin D supplementation in case primary hyperparathyroidism has been unmasked (1)
- adjusted plasma calcium is recommended to be checked one month after completing the loading regimen or after starting lower dose vitamin D supplementation in case primary hyperparathyroidism has been unmasked..the presence of hypercalcaemia ought to lead to cessation of further vitamin D supplementation prior to investigation of the hypercalcaemia
- Vitamin D levels do not need to be checked routinely, and can take 3-6 months to reach a steady state after treatment has started (2)
- recheck vitamin D levels 6 months after a loading regimen of vitamin D has been given. If levels are still sub-optimal, compliance with medication should be discussed. Alternatively, consider referral to an appropriate specialist
Notes:
- dose conversion (2):
- the dose of vitamin D in micrograms can be calculated by dividing the number of international units by 40. Vitamin D2 (ergocalciferol) and vitamin D3 (colecalciferol) are considered equal in potency
- although there are suggestions that the onset of action of vitamin D3
is quicker
- for vegans, vitamin D2 (ergocalciferol) products which are derived
from plants will be most suitable (2)
- however, prescribers will also need to check the formulation of the
product (e.g. some ergocalciferol products will be formulated in a gelatine
capsule, which will be unacceptable to vegans).
- however, prescribers will also need to check the formulation of the
product (e.g. some ergocalciferol products will be formulated in a gelatine
capsule, which will be unacceptable to vegans).
- calcium and vitamin D combined supplements are not routinely indicated
in patients with low vitamin D3 levels unless the patient also has hypocalcaemia.
The calcium component may be unnecessary and can reduce compliance due to
unpalatability. Serum calcium levels should, however, be monitored (2)
- short acting potent analogues of vitamin D such as alfacalcidol or calcitriol
should NOT be used in this situation because there is no evidence to support
efficacy and it can lead to hypercalcaemia
- WARNING: NUT/SOYA ALLERGIES
- vitamin D preparations such dekristol and Fultium D3 contain peanut oil; Drisdol, Calceos and Adcal D3 contain soybean oil. For full details of excipients, refer to individual SPCs
- all patients receiving pharmacological doses of vitamin D should have the
plasma-calcium concentration checked at intervals (initially weekly) and whenever
nausea or vomiting are present (3)
- NOS recommend checking adjusted serum calcium 1 month after completing
the loading regimen or after starting vitamin D supplementation in case
primary hyperparathyroidism has been unmasked (1)
- adjusted plasma calcium is recommended to be checked one month
after completing the loading regimen or after starting lower dose
vitamin D supplementation in case primary hyperparathyroidism has
been unmasked..the presence of hypercalcaemia ought to lead to cessation
of further vitamin D supplementation prior to investigation of the
hypercalcaemia
- adjusted plasma calcium is recommended to be checked one month
after completing the loading regimen or after starting lower dose
vitamin D supplementation in case primary hyperparathyroidism has
been unmasked..the presence of hypercalcaemia ought to lead to cessation
of further vitamin D supplementation prior to investigation of the
hypercalcaemia
- Vitamin D levels do not need to be checked routinely, and can take 3-6
months to reach a steady state after treatment has started (2)
- recheck vitamin D levels 6 months after a loading regimen of vitamin
D has been given. If levels are still sub-optimal, compliance with
medication should be discussed. Alternatively, consider referral to
an appropriate specialist
- recheck vitamin D levels 6 months after a loading regimen of vitamin
D has been given. If levels are still sub-optimal, compliance with
medication should be discussed. Alternatively, consider referral to
an appropriate specialist
- NOS recommend checking adjusted serum calcium 1 month after completing
the loading regimen or after starting vitamin D supplementation in case
primary hyperparathyroidism has been unmasked (1)
- breast milk from women taking pharmacological doses of vitamin D may cause
hypercalcaemia if given to an infant (4)
- vitamin D supplementation is contraindicated in patients with hypercalcaemia
or metastatic calcification
- relative contraindications include primary hyperparathyroidism, renal stones and severe hypercalciuria
- patients with mild to moderate renal failure or known to have mild hypercalciuria
should be supervised carefully when taking vitamin D In patients with
a history of renal stones, urinary calcium excretion should be measured
to exclude hypercalciuria, a problem which requires specialist referral
- assessment of improvement in vitamin D (25OHD) status on replacement
therapy (1)
- routine monitoring of serum 25OHD is generally unnecessary but may be appropriate in patients with symptomatic vitamin D deficiency or malabsorption and where poor compliance with medication is suspected.
- there is considerable variability between the results of studies examining the dose response to vitamin D supplementation, but it appears that much of this inconsistency results from the confounding effects of UV exposure in the summer months. When consideration is confined to the results of studies that examined the effect of supplementation on winter 25OHD levels, the results are more consistent:
- a daily supplement of 20 to 25 µg (800 to 1000 IU) calciferol will cause an increase in 25OHD of 24 to 29 nmol/L. Most of these studies have suggested that a new steady-state 25OHD level is reached by about 3 months and possibly not until 6 months.
- "..accordingly, it is a waste of resources to measure vitamin
D levels too soon after the therapy has started. A minimum of 3 months
treatment must be given and it may be more prudent to wait until 6 months
have passed..."(1)
- specialist supervision in vitamin D supplementation (1)
- if a patient has tuberculosis or sarcoidosis
- patients with granulomatous disease are at risk of hypercalcaemia because of increased 1alpha-hydroxylase activity (which converts 25OHD to active 1,25(OH)2D). Toxicity has been reported during vitamin D treatment of tuberculosis and in patients with active sarcoidosis.specialist advice should be sought before starting these patients on vitamin D therapy
- there may be sub-groups of patients identified who are unable to maintain adequate vitamin D status. These may require a more aggressive replacement or maintenance schedule provided under specialist supervision in a secondary-care setting
- local guidance suggests seeking specialist advice eGFR<30ml/min,
pregnancy, hyperparathyroidism (2)
- if a patient has tuberculosis or sarcoidosis
- recommended daily intake of vitamin D in the UK is around 400IU (10mcg)
for an adult, 280IU (7mcg) for children aged 6 months to 3 years and 340IU
(8.5mcg) per day for infants under 6 months (5)
Reference
- (1) National Osteoporosis Society (2018). Vitamin D and Bone Health: A Practical Clinical Guideline for Patient Management
- (2) NHS Coventry and Warwickshire. Brief Prescribing guide - Treatment of Vitamin D Deficiency in Adults (June 2017)
- (3) CKS Vitamin D deficiency in adults - treatment and prevention. Last revised November 2016. Available at http://cks.nice.org.uk
- (4) Drug and Therapeutics Bulletin 2006; 44(4):26-9.
- (5) http://www.nelm.nhs.uk/en/NeLM-Area/Evidence/Medicines-Q--A/What-dose-of-vitamin-D-should-be-prescribed-for-the-treatment-of-vitamin-D-deficiency/?query=vitamin+D&rank=1