preparations and regimes
Last edited 03/2019
HRT preparations consist of daily oestrogen and with either sequential (cyclic regimen) or daily (continuous combined regimen) progesterone added if necessary (1).
- oestrogen (oestradiol, oestradiol 17β, oestrone, or conjugated equine oestrogen) can be administered orally, intravaginally, or transdermally
- doses are of oestrogen in oral preparations are an order of magnitude greater than the transdermal route. This is because oral preparations are absorbed through the gut and of into the hepatic portal circulation where most of the oestrogen is removed by first-pass metabolism.
- progestogen can be oral, transdermal, or delivered via an intrauterine device (1)
Patches allow absorption of hormones through the skin to the systemic circulation. This pattern of absorption bypasses the liver so there is a more consistent blood level of hormone than via the oral route.
Implants of oestradiol come in doses of 25, 50 and 100 mg and can be inserted into the subcutaneous fat tissues. There are also testosterone implants available which some gynaecologists recommend for improving libido.
In non-hysterectomised women progestogen should be added in for 12 days per month in order to reduce the risk of endometrial cancer. If 12 days are given the daily dose of progestogen can be quite low whereas shorter duration progestogen demands higher doses.
The reason for wishing to have a low progestogen dose is that some women notice progestogen related side effects at higher doses e.g. irritability, breast fullness, abdominal bloating.
A suggested algorithm for prescribing HRT (2) is presented:
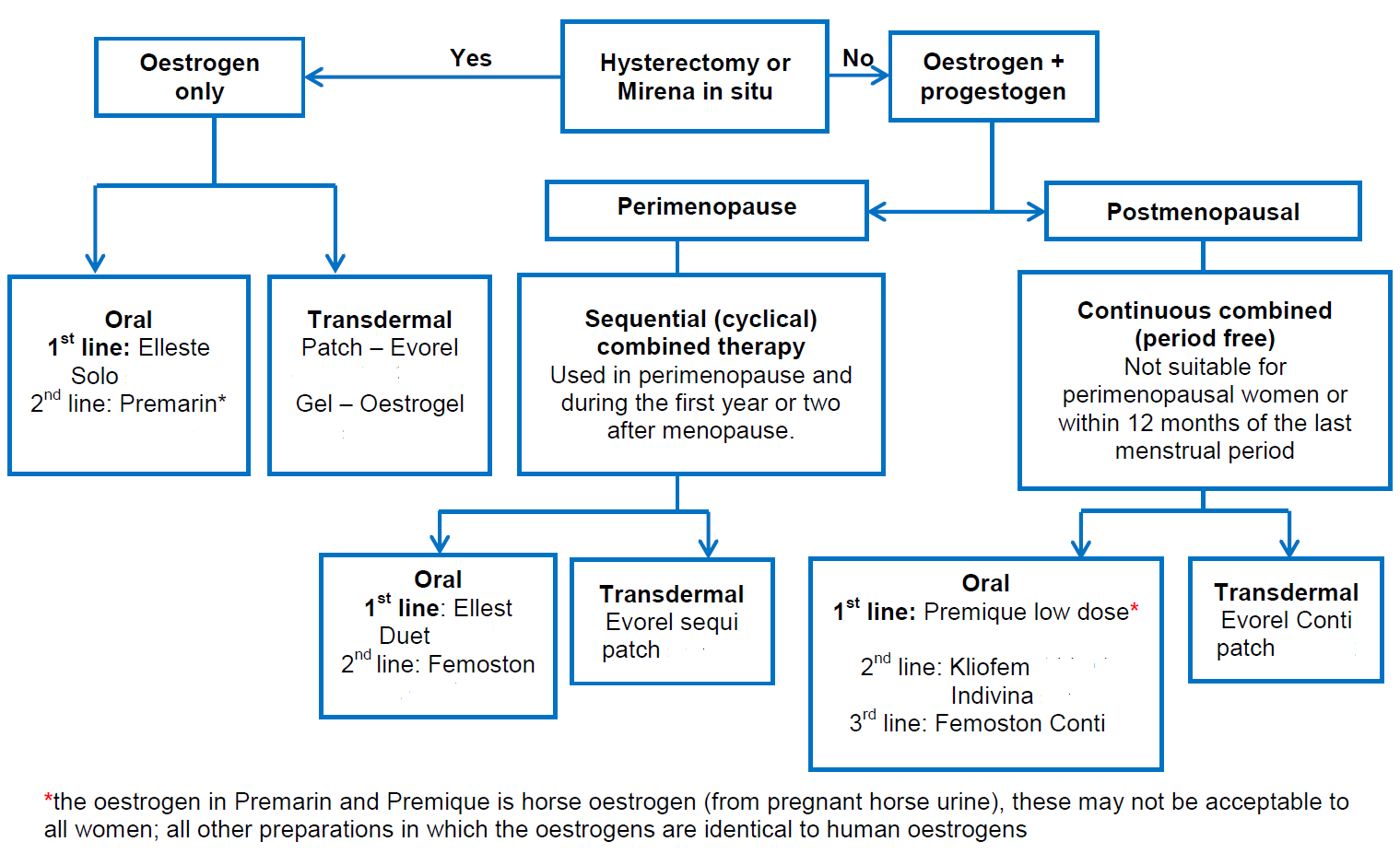
Notes (2):
- choice of HRT
- choice of HRT for an individual depends on an overall balance of indication,
risk-benefit profile, side effects and convenience. Prescribe the lowest
effective dose of HRT for the shortest time possible.
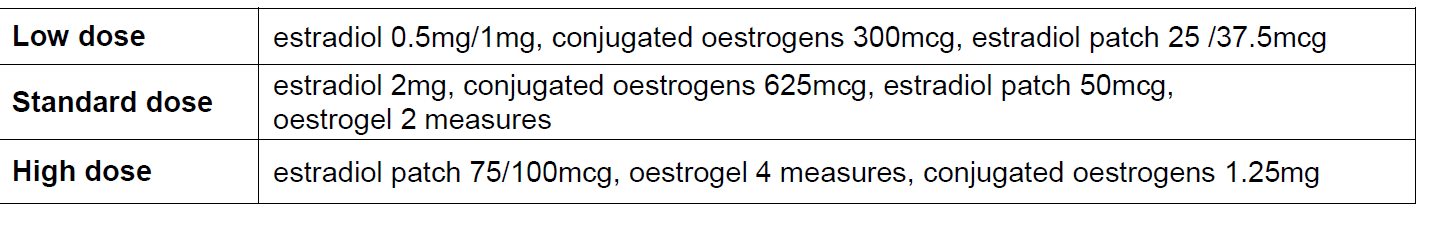
- start at a low dose especially in older women (may be less tolerant of oestrogen) and increase if symptoms persist after a few months. Tailor the dose to the symptoms, as the ingested or applied dose may not be well absorbed
- side effects tend to be related to the progestogen component of combined HRT
- progestogenic side effect may include PMS type symptoms, breast tenderness, lower abdominal pain, backache, depressed mood, acne/greasy skin, headache.
- if androgenic or PMS side effects occur on C19 progestogens (levonorgestrel/norethisterone), advise change to C21 progestogen (dydrogesterone/medroxyprogesterone).
- If side effects are still unacceptable, consider Mirena Intrauterine system.
- choice of HRT for an individual depends on an overall balance of indication,
risk-benefit profile, side effects and convenience. Prescribe the lowest
effective dose of HRT for the shortest time possible.
- Risks associated with HRT (1)
- HRT does not increase cardiovascular (CVS) risk when started under age 60
- HRT is not contraindicated in women with optimally managed CVS risk factors (eg hypertension, diabetes)
- consider transdermal HRT in women with a higher background VTE risk including those with a BMI over 30 kg/m2 as oral HRT is associated with a higher risk of venous thromboembolism.
- HRT with oestrogen (ET) alone is associated with little or no change in the risk of breast cancer, combined oestrogen and progestogen HRT (CET) can be associated with an increase in the risk of breast cancer: however the latter is required in women with a uterus
- Patches versus oral preparations
- patches are more expensive than oral preparations but may be suitable for patients with high risk of VTE (e.g. those with a BMI over 30 kg/m2) - consider referring those at high risk (strong family history of VTE or a hereditary thrombophilia) to a haematologist for assessment before considering HRT
- transdermal routes avoid the first pass effect through the liver and are not associated with increased low density lipoproteins, venous thrombosis or stroke. Patches deliver a more steady level of hormone which can be helpful in conditions triggered by fluctuating levels eg migraine.
Reference:
- (1) Hickey M, Elliott J, Davison SL.Hormone replacement therapy. BMJ. 2012;344:e763.
- (2) Derbyshire Joint Prescribing Committee. Menopause Management Guideline (Accessed 13th March 2019)